Editor's note: Find the latest COVID-19 news and guidance in Medscape's Coronavirus Resource Center.

Kimberly LeBlanc, PhD, RN
Personal protective equipment (PPE) has been essential to protecting healthcare workers from the novel coronavirus, but it presents its own set of challenges to their health, notably skin damage associated with prolonged use of PPE. Medscape spoke with Kimberly LeBlanc PhD, RN, chair of the Association of Nurses Specialized in Wound Ostomy Continence (NSWOC) of Canada, and coauthor of best practice recommendations for preventing and managing PPE-related skin damage.
What's driving the increase in reports of PPE-related skin damage?
Kimberly LeBlanc, PhD, RN: Not only are we using more PPE than we have in living memory, but we are using it in ways that were never intended. Nearly all PPE on the market today is designed for single use. You are supposed to use it and throw it away. Masks were never designed to be worn for more than 4 hours, and certainly not to be worn from patient to patient without being changed.
But we experienced a massive global shortage of PPE so early in the pandemic that people were afraid to dispose of their PPE in case it couldn't be replaced. Nurses were wearing the same PPE for their entire shift, and their skin really suffered as a consequence.
We started getting daily calls from nurses asking for help with these new skin issues. Our evidence summary is based on available research and expert opinion.
How does prolonged PPE use affect the skin of nurses and other HCPs caring for patients with COVID-19?
Almost every type of PPE — face masks, goggles, face shields, gloves — can cause skin problems. Even gowns can cause overheating and profuse sweating, and when combined with friction, that can lead to intertriginous dermatitis.
Hand irritation is especially common when gloves are used with high frequency, as they are now. Not only do the hands become irritated from frequent sanitizing and handwashing, but gloves trap moisture and heat, and the reported effects include contact dermatitis, maceration, and erosion of the epidermis.
We learned about some of these PPE-related skin problems from the 2002-2003 SARS outbreak. A 2006 study from Singapore looked at PPE-related adverse skin reactions in 307 staff members, mostly female nurses. Among those wearing N95 masks, 60% reported an increase in acne, 36% reported a rash, and 51% reported itch or dermatitis.
These effects increase the wearer's risk for infection. If you have any kind of uncomfortable lesion on your face — a new blemish, an itchy rash, an abrasion, or a wound — you are more likely to inadvertently reach up and touch your face or adjust your mask. Every time you do that, you break the PPE protocol and risk contaminating your face.
In the beginning, we were told that SARS-CoV-2 was transmitted by contact with droplets, and that surgical masks were sufficient protection unless you were performing an aerosol-generating procedure, such as intubation or extubation. Very quickly, however, the debate turned to whether the virus was also airborne. People were scared and many started wearing N95 masks all the time.
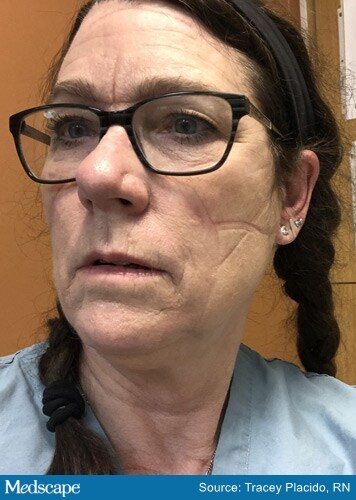
Unlike a disposable surgical mask, the N95 and N99 masks are designed to fit closely against the skin, forming a seal around the mouth and nose. In healthcare settings, these masks (also known as "respirators," which come in different sizes and models) are fit tested on each staff member to make sure they are airtight before they are considered safe and protective. This is important when it comes to options for relieving the pressure of the N95 mask on the wearer's face. Tighter isn't better. When worn for many hours, nurses often have reddened indentations on their faces corresponding to the outline of the mask.

The face of an ICU nurse after removing her mask
Anecdotally, we've heard from nurses who are even having problems with the non-airtight surgical masks. When worn for an entire shift, nurses are getting acne and evidence of skin irritation from pressure or chafing of the mask over the bridge of the nose.
We are also hearing about ulceration on or behind the ears from the elastic loops that stretch around the ears. People have come up with a lot of DIY solutions to relieve the irritation and pressure, such as sewing buttons onto surgical caps or headbands so the elastic can be looped around the buttons, instead of their ears. A mask manufacturer developed, and is providing to hospitals, a thin plastic band with notches that go around the back of the head, and the mask's elastic loops attach to one of the notches on this device rather than the ears.
These creative solutions seem to be working, but care must be taken to avoid making the masks tighter, which will only increase pressure on the scalp and face.
Which is the bigger culprit, pressure or moisture?
It's both. Moisture builds up underneath PPE, including masks, and coupled with pressure, the result is more significant pressure-related skin damage. The dramatic photos posted by HCPs on social media show pressure lines, bruises, and wounds from PPE, and the looks on their faces tell the story. But what you aren't seeing are pictures of nurses with acne flaring from mask use.

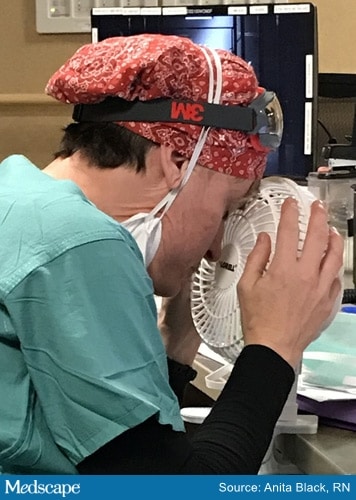
A nurse holds a fan close to cool the hot, painful skin of her face, after removing her soaking wet mask.
With so many different items and combinations of PPE in use, do we have a handle on what causes the most pressure-related skin damage?
We've seen evidence of pressure damage everywhere that PPE makes contact with the head and face.
In a survey of healthcare professionals in China during COVID-19, the most common site of PPE-related skin injury was the nasal bridge, and the most frequent cause of this injury was goggles.
The skin over the nasal bridge is most vulnerable to injury because it is a bony prominence. The skin is thinner with little underlying tissue. Shifting of the mask causes friction and shear, and moisture accumulation contributes to the development of skin damage over time.
The pressure of tight-fitting goggles can be seen around the eyes, cheeks, and nasal bridge upon removal. Most HCPs prefer to wear face shields if they can, but even face shields can cause a band of pressure across the forehead. Many are wearing both.
Ideally, the pressure from a mask or other PPE should be off-loaded periodically, at least every 4 hours. This isn't always possible, unfortunately.
If a clinician is experiencing pressure or irritation, but has no evidence of broken skin, what can be done to prevent adverse skin effects?

Skin indentations from PPE, with intact skin
The field of wound care recognizes four stages of pressure injury, from stage 1 (non-blanchable erythema) up to stage 4 (full thickness skin and tissue loss). We've modified this model for PPE-related skin injury. In our best practices document and educational program, we identify three levels of skin and tissue damage:
* Level 1 is normal, intact skin.
* In level 2, the skin is still intact but it is reddened, indicating some underlying tissue damage.
* The highest, level 3, is non-intact skin of any degree.
The red marks from pressure that commonly appear upon PPE removal are known as reactive erythema (Figure 2) and should show resolution within 20-30 minutes. If the erythema doesn't fade away, it suggests level 2 damage. Do not rub or massage erythematous skin. Non-blanchable erythema suggests that underlying tissue damage has already occurred, and rubbing can exacerbate it.

Skin erythema after removal of goggles and mask
For each of these three levels, we offer a stepwise approach to prevention and management.
Level 1
This is when prevention will be most effective. For both airtight and non-airtight PPE, after washing your face, we recommend moisturizing the skin at least daily with a product of choice. Creams containing acrylate polymers or dimethicone are good options for this because of longer durability. We don't recommend ointments, including zinc. Apply moisturizer to areas of the face that have the most contact with PPE, such as ears, forehead, and nose. Whatever product you use, it must be applied 1 to 2 hours before donning PPE so that it is fully absorbed and completely dry before the PPE is put on. The best time is right after showering or washing your face, at home before you go to work. If you use cosmetics, avoid oil-based foundation. Petrolatum products (such as Vaseline) are likewise not recommended.
Then, 5 minutes before applying goggles or mask, apply an alcohol-free skin barrier wipe (also known as liquid skin protectants or sealants) to your face, covering the areas most likely to be affected by PPE (the "T-zone"), avoiding the eyes and mouth. Allow this to dry for 1 minute so that it is no longer tacky to the touch before donning PPE. Many different brands of alcohol-free skin barrier products are available; we don't recommend using a spray on the face because it's hard to control where it goes.
As much as possible, HCPs should remain hydrated for general skin health.
Level 2
For HCPs with non-blanchable erythema, but with skin still intact, the recommendations are the same. Use a moisturizer, allow it to dry, and apply a skin barrier wipe before donning PPE. The type of mask being worn should dictate a decision about use of any additional dressing between the skin and mask. Note that the skin barrier wipe will reduce shearing, but it won't alleviate pressure.
Underneath surgical masks, a dressing of some type can be used to cushion the skin from the pressure of the mask. Options include a thin adhesive foam dressing, a silicone adherent sheet (perforated or nonperforated), and a thin hydrocolloid sheet. Whatever type is used, it should be as low-profile as possible, and cut to cover the desired area (patterns for cutting these dressings can be found in the best practices document, along with other tips about application, assessment, and removal of dressings).
Underneath N95 masks, a dressing could interfere with the effectiveness of the mask by disrupting the airtight seal. Therefore, before applying a dressing, the HCP should check with the facility's health and safety department for approval and arrange for fit testing with the dressing in place. If use of a dressing is approved, use a thin, low-profile, semi-occlusive dressing.
Level 3
HCPs with areas of non-intact skin should follow the same routine for preventive skin care, and follow the recommendations for the use of dressings under the mask. If open wounds are present, some type of dressing might be necessary.
We also don't recommend the use of topical skin adhesives or glues. They can be difficult to remove.
Once the skin is broken, it is unlikely to heal if the HCP continues working in the same area and wearing the same PPE. Few nurses have enough days off between shifts for their skin to fully heal, and even if it does, it's very fragile and will break down again when the nurse goes back to work.

Points of skin pressure with wounds caused by a mask
Nurses need to speak up to their managers and health and safety supervisors. Show them what you are going through. Show them your face. You are the walking wounded.
Can you recap the skin care sequence you recommend for nurses and other HCPs who must wear PPE at work?
Sequence:
1. At home (before you leave for work or 1 to 2 hours before you will be donning PPE):
2. At work, before donning PPE:
Apply skin barrier wipe to dry face: forehead, nose, cheeks, ears (if needed)
Let dry 90 seconds, until no longer tacky
3. Don PPE.
Your educational program mentions that HCPs who have preexisting skin conditions may find that these are exacerbated by PPE use. Can you explain?
Frequent skin cleansing causes dermatitis of the hands of many nurses — reddened, painful, itchy even bleeding skin on the back of the hands. This type of occupational skin injury often occurs in HCPs, especially during the winter. Frequent handwashing and glove-wearing can result in breaks in the skin, which then serve as another entry point for the virus.
Nurses who are prone to such skin conditions as eczema or psoriasis are reporting more problems now as a result of repeated handwashing and glove wearing.
If you don't take care of your skin, you are going to have skin breakdown.
Laura A. Stokowski, RN, MS, is the editor of Medscape Nurses.
Kimberly LeBlanc PhD, RN, NSWOC, WOCC (C), IIWCC is Chair, Wound Ostomy Continence Institute of the Association of Nurses Specialized in Wound Ostomy Continence Canada.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.