High doses of docosahexaenoic acid (DHA) supplements may help prevent progression to dementia in people who carry the apolipoprotein ε4 allele (APOE4), a new review suggests.
The hope is that this new review of current evidence will spark renewed interest in funding research into DHA in APOE4 carriers, said lead author Hussein N. Yassine, MD, assistant professor, endocrinology, Department of Medicine, Keck School of Medicine University of Southern California, Los Angeles.
"What we are trying to say is that maybe we should invest more in studies looking at DHA in the right population," said Dr Yassine.
Their report was published online January 17 in JAMA Neurology.

Dr Hussein N. Yassine
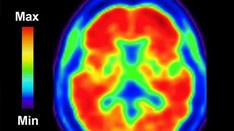
DHA is an essential long-chain omega-3 polyunsaturated fatty acid found in fish, as well as in the brain, liver, and elsewhere in the body. It plays a role in the formation of synapses and indirectly limits the production of amyloid deposition and helps cells clear toxic amyloid peptides.
Having the APOE4 allele is one of the strongest risk factors for developing Alzheimer's disease (AD). This allele is present in 20% of the general population but in about 50% of patients with AD.
Researchers searched the PubMed database for original articles, systematic reviews, and meta-analyses of omega-3 studies in AD that were published before August 30, 2016. They selected preclinical studies, cross-sectional studies, longitudinal cohort studies, and randomized clinical trials (RCTs).
Research in animals is quite clear. Studies have shown that mice or rats given enough DHA over at least 10% of their lifespan don't develop AD pathology (amyloid) in the brain, said Dr Yassine.
"And if you take a particular kind of AD mouse model — the human APOE4 mouse model, which have the human APOE4 gene inserted — and give them high doses of DHA for a long time, beginning when they're young, you can prevent features of AD."
Some observational studies in humans also link DHA consumption to lower risk for AD. In his review, Dr Yassine referred to a meta-analysis by Zhang et al that summarized 21 studies of 181,580 participants with 4438 dementia cases identified during a follow-up ranging from 2.1 to 21 years.
That analysis found that compared with not eating fish, consuming 1 serving of fish per week was associated with a significantly lower risk for AD dementia (relative risk, 0.93; 95% confidence interval, 0.90 - 0.95; P = .003).
Interestingly, increasing fish consumption to two, three, or more servings per week "doesn't make a huge difference," said Dr Yassine.
He and his colleagues also looked at 14 RCTs to address the question of whether fish oil supplements are effective in AD. "The answer is clearly no," said Dr Yassine. While some studies suggested that the supplements may have some impact in cognitively normal subjects, "If patients have AD, fish oil doesn't do anything." That is likely because AD neurodegeneration cannot be reversed with fish oil supplements.
However, the picture looks different in people with APOE4 who haven't yet progressed to dementia. In some epidemiologic studies and clinical trials, there's a trend of cognitively healthy APOE4 carriers benefiting from taking fish oil supplements over an extended period of time.
Dr Yassine discussed the Rush Memory and Aging Project, in which participants free of dementia underwent annual clinical neurologic evaluations and brain autopsy at death. After a mean follow-up of 8 years, that study showed APOE4 carriers who consumed at least one meal of seafood per week had fewer AD neuropathologic changes compared with those who consumed less fish.
Several possible mechanisms might link APOE4 with DHA metabolism, the authors note. These include accelerated liver catabolism of DHA; defective DHA transfer across the blood-brain barrier; and hypolipidated or decreased APOE4 particle numbers, resulting in less efficient brain DHA metabolism.
"Evidence supports the contention that these APOE4 mechanisms operate before the onset of neurodegeneration," they write.
Dr Yassine would like to "stimulate interest" in further studies of DHA in APOE4 carriers. However, he recognizes that funding for such research is difficult to come by. Pharmaceutical companies don't see this as a cost-effective area, and the National Institutes of Health has already funded a large study that turned out negative.
Some believe, said Dr Yassine, that DHA has been investigated enough and "it's time to move on."
But he pointed out that the Alzheimer's Disease Cooperative Study–funded DHA trial included patients with neurodegeneration. "We now know that once the nerves are dead, DHA is not going to make them come alive again."
Dr Yassine is convinced that new and properly done investigations in the right population will likely provide more evidence that DHA supplements "are a cost-effective and safe" way to prevent AD.
Mixed Results
The review is "very complete," providing an overview of all observational studies and RCTs investigating the role of omega-3/DHA intake or levels with AD and cognitive decline, commented Ondine van de Rest, PhD, University of Wageningen, the Netherlands, who has done research in this field but was not involved in the review.
The conclusion from observational studies that a serving of fish once a week fish reduces AD risk is useful, she noted. "Fish once per week is for many people quite feasible to achieve, so that is a nice public health message."
Dr van de Rest noted that the review authors separated clinical trials by target group, for example, by participants with AD or mild cognitive impairment and those who are cognitively healthy. "This is relevant, since it appears that DHA supplementation is no longer effective in patients with AD, but is effective in people with mild cognitive complaints."
Results of observational studies that assessed the relationship between omega-3 intake and cognitive outcomes by APOE4 status are mixed, with about half finding an association between omega-3 intake in noncarriers and the other half finding associations in carriers, said Dr van de Rest.
But most (three of four) of the RCTs found effects of omega-3 supplementation in APOE4 carriers, she noted. "The authors draw their main conclusions based on the trial results: supplementation with DHA is effective in APOE4 carriers, and then before the onset of AD."
"My personal view is that, even though the majority of randomized controlled trials showed effects of DHA in APOE4 carriers, this evidence is mixed from observational studies. Therefore, I would first still like to see results of more studies performed in both carriers and noncarriers, because it is not ultimately clear yet that the effect of DHA/fish intake is limited to carriers only."
Dr Yassine has disclosed no relevant financial relationships.
JAMA Neurol. Published online January 17, 2017. Abstract
Medscape Medical News © 2017 WebMD, LLC
Send comments and news tips to news@medscape.net.
Cite this: DHA Supplements Linked to Less Progression to Alzheimer's in APOE4 Carriers - Medscape - Feb 03, 2017.










Comments