History of Cataract Surgery
Cataract surgery is one of the oldest surgical procedures known, first documented in the fifth century BC.[12] In ancient times, cataracts were treated with a technique called couching, which could only be performed when the lens had become completely opaque, rigid, and heavy to the point that the supporting zonules had become fragile. The eye would then be struck with a blunt object with sufficient force to cause the zonules to break so that the lens would dislocate into the vitreous cavity, restoring limited but completely unfocused vision. Centuries later, the technique was modified so that a sharp fine instrument was inserted into the eye to break the zonules to cause the dislocation.
The first reported surgical removal of a cataract from the eye occurred in Paris in 1748.[13] The advent of topical anesthesia made this procedure more practical. The early techniques involved removing the entire opaque lens in one piece using an incision that went halfway around the circumference of the cornea. It was critical that the lens remained intact as it was being removed, so surgery was restricted to so-called ripe lenses: cataracts so hardened that they would not break into pieces as they were being removed. This limited the surgery to only the most advanced cataracts. Since fine sutures did not exist at that time, patients were kept immobilized with sandbags around their head while the wound healed. Consequently, the early literature reporting cataract surgery routinely documented the mortality rate (secondary to pulmonary emboli).
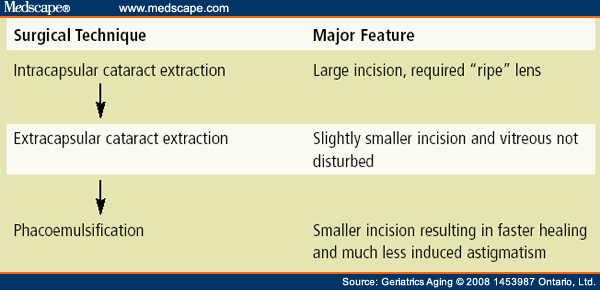
The improvements in cataract surgery and the corresponding results over the past few decades have been nothing short of astounding ( Table 1 ). The first major advance was the development of techniques allowing the removal of the lens while leaving the lens capsule behind.[14] The intact capsule acted as a barrier preventing lens material from falling into the vitreous cavity. This allowed less advanced cataracts to be removed since any residual fragments could be removed at the time of surgery with aspiration and would not be retained in the vitreous, where they would incite inflammation. This change also resulted in the reduction of the wound down to approximately a quarter of a corneal circumference. The introduction of fine sutures around this time greatly enhanced the safety and quality of results.
The most significant change marked by the modern era was the introduction of phacoemulsification surgery in 1967 by Dr. Charles Kelman.[15] In this technique, ultrasonography is used to break the lens into minute fragments that can be aspirated. A combined ultrasonographic, irrigation, and aspiration hand piece allows the removal of any lens through a small incision. This revolutionized the performance of surgery, leading to smaller and smaller wounds. Today, routine wounds are <3 mm long, and 1 mm wounds are on the horizon.
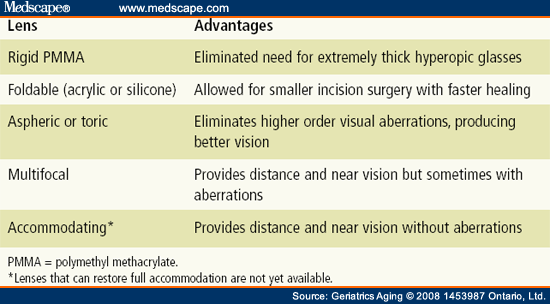
As the evolution of surgical techniques progressed, the advancement in lens replacement technology was equally dramatic ( Table 2 ). Originally, no intraocular lens implants were used following cataract surgery, and patients had to rely on “Coke bottle”-thick hyperopic glasses. These were associated with a variety of unpopular optical aberrations. Intraocular lenses evolved secondary to the pioneering work of Howard Ridley, a British ophthalmologist.[16] He recognized that the penetration of shattered fragments from airplane windshields into the eyes of World War II fighter pilots when their planes had been hit did not always lead to damage. He created the first artificial lens from this material, leading to the creation of an entire industry.
The evolution of smaller surgical incisions was matched by the development of new lens implants created out of different materials (such as acrylic and silicone) that could be folded to allow the lens to be inserted through a tiny wound. At the present time, commercially available lenses can be inserted through wounds a little over 2 mm.
Lenses are manufactured in a variety of different optical powers. Prior to surgery, patients undergo a series of measurements determining the optical length of their eye and the focusing power of their cornea to determine what will be the optimal intraocular lens power for them. The majority of the lenses currently implanted in North America are monofocal with a power chosen to restore good distance vision. This usually still leaves the patient dependent on glasses for reading.
A recent advance has been the creation of aspheric lens technology that not only corrects the patient's focal length but also corrects some optical aberrations that naturally occur in the cornea due to aging.[17] The prime goal for lens developers in recent years has been to create a lens that will restore quality distance and near vision without the need for glasses. The initial attempts involved the creation of multifocal lenses that have concentric rings of different optical strengths so that light from different distances is focused on the retina. These complex lenses are associated with some optical aberrations that are not always tolerated. This has led to limited adoption of these lenses in North America.
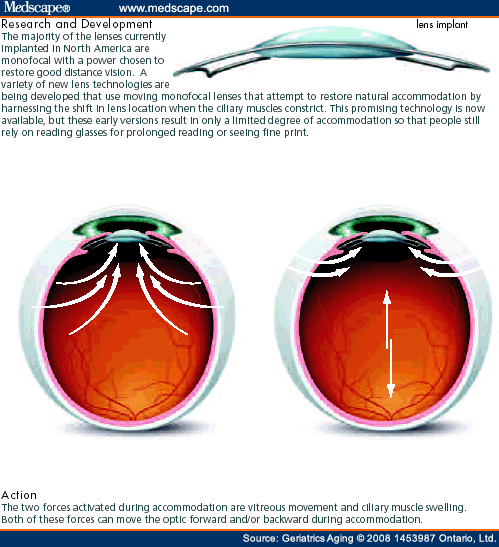
A variety of new lens technologies are being developed that use moving monofocal lenses that attempt to restore natural accommodation by harnessing the shift in lens location when the ciliary muscles constrict (Figure 2).[18] This promising technology is now available, but these early versions result in only a limited degree of accommodation so that people still rely on reading glasses for prolonged reading or seeing fine print.
Figure 2.
Accommodating Lens Implant
As these basic lens technologies have given us the ability to correct hyperopia or myopia, treatments have developed to also deal with preoperative astigmatism (irregularity of curvature of the cornea). A popular approach uses limbal relaxing incisions[19]; this approach involves making almost complete-thickness cuts through the peripheral cornea at the appropriate location to neutralize the astigmatism. As excimer laser technology has improved, some surgeons have elected to use this procedure to correct residual astigmatism as well as any residual hyperopia or myopia that remains following the cataract surgery.[20] This is the principal use of this laser technology among older adults since this technology is primarily aimed at young patients seeking to eliminate myopia. Finally, new intraocular lens implants are now available that can correct not only myopia or hyperopia but also a variable degree of astigmatism.[21] These lenses come with a variety of astigmatic powers. When they are implanted, the surgeon simply lines up the surface markings of the new lens with the previously measured steep access of the patient's astigmatism to neutralize it.
Geriatrics and Aging. 2008;11(6):328-332. © 2008 1453987 Ontario, Ltd.
Cite this: The Evolution of Cataract Surgery: The Most Common Eye Procedure in Older Adults - Medscape - Jul 01, 2008.





Comments