E. Magnus Ohman, MD : Hello . I'm Magnus Ohman. Welcome to another edition of Life and Times of Leading Cardiologists. We are very fortunate to have a great contributor of science in cardiovascular medicine, Prof Gilles Montalescot. He is from Paris and Sorbonne University, which is world-famous, of course. Welcome.
Gilles Montalescot, MD, PhD: Thank you very much. It's wonderful to be here.
Dr Ohman: You have had a very distinguished career, mostly focused around thrombosis, and we will talk a little bit about that later. Many of us have wondered: Where did Gilles come from and where did he grow up?
The Journey Begins in Paris
Prof Montalescot: I was born and raised in Paris—a nice city to grow up in. Actually, my family originates from the center of France, from what we call Limousin, which is in Périgord. It's a region of lakes and forests.
Dr Ohman: Famous for truffles?
Prof Montalescot: It's famous for truffles and mushrooms. It's kind of a wild area. The name "Montalescot" comes from the name of a village, and the family comes from here. Actually, my grandfather was in Périgord, and the first one to move to Paris was my father. My grandfather was a small farmer—two or three cows, one pig, and cultivating a few acres, and trying to survive in this region. After World War II, my father went to Paris and started working in Paris. No qualification, no diploma.
He became an employee of the French Railway Society. His job was to use big hammers to hit wheels on the trains just to make sure there were no faulty wheels, because if there was a faulty wheel, the train could not leave. That was his first job, but he had many others afterwards. The railway station was next to Pitié-Salpêtrière Hospital.
Dr Ohman: Where you are now practicing?
Prof Montalescot: Exactly. Just behind the walls of the highway station from the hospital is the nursing school where my mother went.
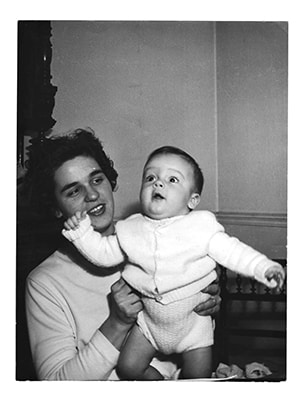
An infant Montalescot with his mother.
Image courtesy of Prof Montalescot
Dr Ohman: Your mother was a nurse? You keep it very small, like on the farm. That is pretty good. Do you have brothers and sisters?
Prof Montalescot: I have a younger sister who lives in Marseille in the south of France. She works for a state organization allocating low-rent flats [apartments] to people with a low income.
Dr Ohman: That is a very honorable thing to do. So, you grew up in Paris.
Prof Montalescot: We lived in a suburb of Paris, close to the Marne River, and we had a happy life there. Our family was not poor, but not rich either. We had a nice living, with family values.
Dr Ohman: You were growing up in the '60s, I take it? There were some demonstrations in Paris, I remember.
Prof Montalescot: Yes. I was a little too young for that. My father did not like me to be outside in the manifestations, so I was not really part of it.
Education Was Very Important
Dr Ohman: Did they keep a studious check on you so that you focused on academics?
Prof Montalescot: Yes; education was very important at home. My father did not go to high school or to the university, so we could not miss school. We could not mess up at school. Education was part of life for my sister and me. We had to be good at school and we were checked on by my father.
Dr Ohman: Being a nurse, did your mother bring the topic of medicine to the household?
Prof Montalescot: Not really, but I remember that when she used to work on Sundays, my father, younger sister, and I would wait for her in front of the hospital door to come out.
Dr Ohman: You saw doctors coming out.
Prof Montalescot: Exactly. It started very early. Later, when I was a teenager, I went to the hospital where she was a nurse in the emergency room. I looked at all of the people waiting for care and all of the white coats trying to help the people. This was a fascination for me.
Dr Ohman: Fast-forward 30 years later or even more: You have been talking extensively about time-to-treatment for care of acute myocardial infarction. It's interesting how that came back. You finished your baccalauréat, the French high school degree. Did you go straight to medical school?
Prof Montalescot: I realized in the last year of high school that I would love to go to medical school. I went to the university and then started my medical studies.
Dr Ohman: The French system is competitive, am I correct? It's hard to get in, but once you are in, you are sort of set.

A very young Montalescot.
Image courtesy of Prof Montalescot
Prof Montalescot: Exactly.
Dr Ohman: Obviously your mother was a large influence, but was there anyone else during that school time who said you would be good at science?
Prof Montalescot: No. I am the first doctor in the family, and probably the last one too. My children will not go into medicine. I'm very happy to be a doctor, to be a cardiologist. Clearly, I think unconsciously my mother had a big influence on this decision.
Medical School, Residency, and an Important First Patient
Dr Ohman: Which medical school did you go to?
Prof Montalescot: A medical school in the suburb of Paris, in Créteil, as the French people would know. It is a very good medical school and I had a lot of mentors there. That was a good time.
Dr Ohman: Once you finished medical school, were people saying, "You should be a surgeon"? It was a big class, too—700, probably?
Prof Montalescot: I was attracted to cardiology quite rapidly. The first day I was a resident, my first patient was the chief of cardiology.
Dr Ohman: We are here at the American Heart Association (AHA), where the president of AHA had a heart attack, so none of us are protected. Interesting. Tell me what happened. Your chief of cardiology comes in with a heart attack.
Prof Montalescot: Yes. He was hospitalized in the first room of the cardiac care unit (CCU) in his own department. That was in 1981.
Dr Ohman: We had CCUs, but nothing else really in care, right?
Prof Montalescot: Aspirin, heparin, beta-blockers—that was about it.
Dr Ohman: Were you the intern?
Prof Montalescot: Yes. I was afraid to go into the room and start my first prescription of residency. He helped me. He told me, "I'm going to tell you what you should give me."
Dr Ohman: This is a wonderful patient. Let me take care of you. Presumably he did okay?

Montalescot in the cath lab between cases.
Image courtesy of Prof Montalescot
Dr Ohman: Then you were set in cardiology. Did he help you get your next job?
Prof Montalescot: Yes, he did okay.
Prof Montalescot: Yes. Prof Hatt (that was his name) helped me a lot. I was a strong researcher also, so from the first day, I was in clinical and basic research in cardiology.
Dr Ohman: How do you specialize after this? Do you do your residency and then your cardiology training?
Prof Montalescot: Yes. It's a 5-year program, and you have to spend at least half of it in cardiology. You specialize in cardiology and then you can move on. Interventional cardiology can become, as it was in my case, an important feature of your residency. It was also my decision to go into the cath lab.
Basic Research, Boston Style
Dr Ohman: You were involved in some basic research in the cardiology sphere before all of this interventional business. What were you doing?
Prof Montalescot: Basic research is usually the first step in research that we have to do. I started with Prof Hatt and then went on with others in other places. I was very much interested in prostaglandins. When I came to Boston for a year of fellowship, I studied thromboxane and prostaglandins.
Dr Ohman: Was this towards the end of your fellowship or in the beginning?
Prof Montalescot: Immediately after my fellowship in cardiology.
Dr Ohman: Where did you go in Boston?
Prof Montalescot: I went to Massachusetts General Hospital and worked with a physiologist, Warren Zapol, who was a mentor and a very nice man. I had a great time spending a year in Boston, studying thromboxane and prostacyclin and the effects on the vasculature.
Dr Ohman: Prostaglandins have something to do with the platelets. Obviously, this shaped the rest of your career because you have been an absolute leader in this. How long were you in Boston?
Prof Montalescot: I was in Boston for a year in the late '80s and then went back to Paris to continue with cardiology.
Dr Ohman: How was it coming from Paris, the City of Lights, to Boston?
Prof Montalescot: Boston is probably the most European city you have in the United States, so it was perfect for me.
Dr Ohman: You survived us, then.
Prof Montalescot: Yes. I lived on Beacon Hill, close to the hospital. That was fun and I had a good time there.
Dr Ohman: That's great. At this stage, were you married?
Prof Montalescot: I was just married, but my wife was a teacher and had to stay in Paris. She would come to Boston several times a year.
Dr Ohman: She could not get a leave of absence?
Prof Montalescot: No; that was a part of the fellowship. My wife was in Paris and I was in Boston, but we made it.
Dr Ohman: Did you work hard in Boston?
Prof Montalescot: I worked very hard and I enjoyed it. I got my first paper in Circulation.[1,2]
Dr Ohman: Your first paper was in Circulation?
Prof Montalescot: Yes. That was a good start.
Au Revoir, America--Back to Paris and Family
Dr Ohman: Now you are back in Paris. Had you finished your interventional training at this stage?
Prof Montalescot: I continued and went to the cath lab. I started to go to the cath lab during my residency, of course, but I became an interventional cardiologist afterwards.
Dr Ohman: Were you able to integrate what you learned about prostaglandins in Boston with the percutaneous coronary intervention or angioplasty we were doing in those days? It was pretty crude.
Prof Montalescot: Yes. I used what I had learned in Boston in Paris and looked at the relationships between thromboxane, platelets, vasoconstriction, and thrombus. We had a couple of papers at the time about samplings of blood in the coronary sinus in these coronary patients during angioplasty.[3,4]
Dr Ohman: How was it possible for you to integrate—I would now call that translational research—into the practice of medicine? This is what everybody is worried about now, but you did it. Was it easy, was it hard?
Prof Montalescot: I think it's easy. I had a curiosity and hypothesis and said, "Can we answer this question?" With my colleagues, we tried to answer the question, we published the results, and then we went on to clinical trials. It's always the same thing—you need to be curious, have a question, and design a study to answer the question,
Dr Ohman: You designed a few trials through the years. Let's back up to your family. You were married to a teacher. She was left behind while you were in Boston working hard for a year. Do you have children?
Prof Montalescot: Yes, three children. Two daughters, who have left home now, and one boy. My son is 14 years old and I do not know what he will do, but he says he will never be a doctor.
Dr Ohman: My oldest son said, "Dad, you work too hard. All of the neighbors work less than you. I'm not going to go into that." Now he works harder than I do [outside of medicine]. You never know.
Prof Montalescot: We will see.
Trials in Cardiology
Dr Ohman: You did some of the most impactful trials that we have had in this field, such as the early glycoprotein IIb/IIIa receptor blocker and a number of studies in genetics. How did you make the switch from translational medicine into testing a hypothesis?
Prof Montalescot: It's the same way of thinking. When you treat patients, sometimes you have an unanswered question and it becomes a hypothesis. You start thinking, "Can I try to answer this question?" And you set up a clinical trial. The first one, ADMIRAL,[5] was published in the New England Journal of Medicine. It was not a big clinical trial and only had 400 patients.
Dr Ohman: Your first-ever publication was in Circulation and your first trial was in the New England Journal of Medicine. It would be very hard to beat this.

Montalescot checks his phone before giving a talk (advertised above) at an international conference.
Image courtesy of Prof Montalescot
Prof Montalescot: Yes, but if the question is important and you find an important answer to the question, you can make it into a good journal. That is the way it happened.
Dr Ohman: Have you been able to maintain the basic science component of this? I suppose genetics is a little bit about that.
Prof Montalescot: Platelet function, for example, has become a major subject of interest in our clinical trials. We performed ARCTIC[6] and ANTARCTIC[7] afterwards, trying to monitor the platelet function in these coronary patients and trying to adjust treatment on the basis of platelet function. It did not work, but we tried. In many clinical trials we did substudies to better understand the things we were doing. Yes, you can combine both basics and clinical research.
Memorable Mentors
Dr Ohman: Besides your first patient, Prof Hatt, who were the mentors throughout your career that you really admired and helped you get to where you were going?
Prof Montalescot: It's going to be a couple of French names, of course. Prof Grosgogeat at Pitié-Salpêtrière Hospital told me one day, "You should work on thrombosis. This is going to be very important."
Dr Ohman: How did he get that insight?
Prof Montalescot: I do not know; I did not believe him. He was right and it was a brilliant idea. Prof Thomas, a fantastic clinician, and Prof Rapin in Créteil, who was in charge of the ICU, helped me find my way in cardiology.
Family and the Future
Dr Ohman: You alluded to your daughters, who presumably are not in medicine, based on what you said, and we have your undeclared son. What do your daughters do?
Prof Montalescot: My older daughter is a psychologist.
Dr Ohman: That is close enough to cardiologist.
Prof Montalescot: That is close but she did not want to go to medical school. She could have done it but decided otherwise. My second daughter works in a restaurant—so totally different.
Dr Ohman: That's great. Where do you go from here? You have been one of the most successful leaders worldwide on platelets and thrombosis. What is next for Gilles?
Prof Montalescot: There are still a few clinical trials we want to do, and the idea now is to build a team able to conduct all of these clinical trials. They must not be "my" clinical trials. There is a team around me. I'm the head of the cardiology department now and I want the younger colleagues to be able to do the same thing. With most of the recent clinical trials we have performed, when you look at the publication, the first name is always someone from my team, Jean-Philippe Collet, Johanne Silvain, and others. Clearly, they can shape the future with these new clinical trials.
Taking on the Government
Dr Ohman: I recall that you took on the French government about regulations in clinical trials. That is a fairly large task, even though you have a new president who might help things along a little bit. That is an unusual career path to take on. What possessed you? What went into that decision-making?
Prof Montalescot: Yes, it's a funny story because I did not want to enter politics. But I had to go to the Ministry of Health and defend the clinicians and those doing clinical research because there was a big issue with where the money should go. This money for clinical research should go to the places and people doing the research and not the administrative people. That was the struggle and we won that fight. I'm very glad for all of my colleagues.
Dr Ohman: Congratulations. That is a great success story. Most of us do not take on the government and win, so that is highly successful.
Finally, About That French Food and Red Wine...
Dr Ohman: We have had about a 20-minute discussion with a French man and have not talked about good food and wine. Is the French paradox correct? Can one eat and live very well in France and not have coronary disease?
Prof Montalescot: There is coronary disease in France, but you can eat and drink well and still avoid it. We are quite lucky. We probably have better genes in France than anywhere else. We also have good food and good wine, which are probably protective also. We know that nuts, for example, are very healthy and red wine is also part of prevention.
Dr Ohman: Cardiologist to cardiologist: Do you have wine every evening?
Prof Montalescot: Probably not every day, but quite often. I like it and it's a real pleasure to share a bottle of wine with a friend.
Dr Ohman: It's fascinating to hear this. I'm relieved that the French paradox may be genetically driven because I worry about our US colleagues eating foie gras and other French foods, and thinking that they are cured when they are not. You have been great to share a lot of interesting things with us, Gilles. Thank you very much.
Prof Montalescot: Thank you very much for having me.
© 2018 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Life and Times of Leading Cardiologists: Gilles Montalescot - Medscape - Jan 18, 2018.











Comments